Healthcare design in a post Covid-19 world

Nick Fairham, Principal at global architecture practice BDP, examines how we can change healthcare design in the future and how flexibility of space is key to this success.
The Covid-19 pandemic has resulted in a marked change to the way healthcare is delivered in the UK. Here at BDP we were involved in drawing up plans for six emergency Nightingale hospitals in England and Wales, converting stadiums and conference centres to temporary hospitals. The pandemic has seen outpatient facilities being delivered virtually for the first time as well as the need for many more testing laboratories across the country. As professionals in healthcare design we have had to adopt new ways of working and it has become more important than ever to collaborate closely with clinicians when we are designing healthcare facilities to ensure that they are fit for purpose. The result is complex projects being delivered in record time.
The Nightingale hospitals are not, however, permanent. From a healthcare design perspective we need to be in a place where the NHS can potentially comfortably deal with Covid patients and yet still endeavour to deliver a “normal service” in a hospital. Flexibility in future hospital design is therefore crucial.
Reconfiguring the current space
The ideal scenario would be that if a region is experiencing a spike in Covid cases, the design of the hospital in that area would be able to react accordingly. So for example, outpatient space, which is increasingly being delivered virtually, could be reconfigured to increase diagnostic and treatment capacity. Likewise, the current home-working trend could also generate capacity in existing admin spaces, allowing soft space to be used to accommodate increased capacity and assist in the re-organisation of sites for the HIP (Health Infrastructure Plan) programme. This is a real opportunity for the healthcare sector because with much more bed space, discrete areas can be created for Covid patients within existing facilities. This would result in the infection being controlled and enable the rest of the hospital to carry on as normal.
If hospitals are to achieve this goal, streamlining patient flows will become essential in healthcare design. One possible scenario is creating triage points in admission areas so that those infected with Covid-19 would be separated from others at the outset. Zones would be colour-coded: blue for Covid-infected patients, green where you can be reasonably certain nobody is infected, and amber where it is still not known. This would address clinical needs more efficiently and also give the wider public confidence that it is safe to use emergency services again.
Designing new spaces flexibly
Any new hospital or clinical space should be designed flexibly so that it can potentially have multiple uses over its lifespan.
Standardisation is a key best practice to achieve this. When BDP designed Southmead Hospital in North Bristol NHS Trust (pictured above), rooms were loose fit with services provided to accommodate multiple functions and arranged in defined clusters. Scenario testing showed that major items of equipment could be replaced with minimal reconfiguration, giving operational flexibility over the life of the building.
Minimising patient movement
Clinicians agree that once patients are admitted to hospital, particularly with a highly contagious virus such as Covid-19, reducing patient transfers around the hospital is essential to keeping infection rates low. Healthcare facilities should be designed with more acuity-adaptable patient rooms. These allow every stage of patient care – from admission to discharge – to be delivered in one place and improve operational flexibility. Such rooms cannot unfortunately be achieved through converting four bed bays due to the amount of equipment and space needed to nurse patients.
Whilst nested en-suites can achieve this to some extent, a new approach at the design stage is needed to allow for a much larger area for each room. Of course, this impacts on cost and space but in a post-Covid era there may well be more enthusiasm for this approach to curb future infection rates.
Designing new stand-alone facilities
Patient backlog in planned care has been well documented in recent months so a new approach in healthcare design is needed to help tackle this. One solution is to use planned care centres which can be achieved through new facilities which offer a highly efficient throughput of patients without risk of disruption via unplanned cases (or Covid-19) or process redesign in existing facilities.
Heatherwood Hospital, currently under construction in Ascot, Berkshire, will include six theatres for elective surgery, 48 inpatient beds and 24 day-case cubicles, outpatients (and imaging), with endoscopy. The outpatient space will also be able to be used flexibly with rooms that can accommodate different uses and depending on how many virtual appointments are being used.

Digital technology will allow the planning of one-stop shops, where consultation, testing and diagnostics can be arranged on the same day to avoid repeat visits for Urology and Breast Care patients.
Valuing and protecting staff
The most valuable asset to any organisation is its staff and in the face of the Covid-19 pandemic, it’s more important than ever that NHS staff feel looked after and valued. Creating spaces where staff feel truly valued is an important part of this. Southmead Hospital’s rooftop restaurant is a good example of this. It offers informal networking, break-out areas and meals with a dedicated roof terrace. The masterplan of the hospital also offers active travel routes and spaces designed for cycling, walking or reflecting which has resulted in many more staff choosing to cycle.

From virtual to reality
Finally, as we consider the future of healthcare design and, in particular, the importance of creating flexible space, technology should be used to bring a design to life at the earliest stages of the process. To add real value to business case optioneering healthcare providers should be able to use 3D visualisation to test out different scenarios and how they could play out in a design space. Highlighting the importance of collaboration from the start, adaptations and improvements can then be implemented before a project goes to site.
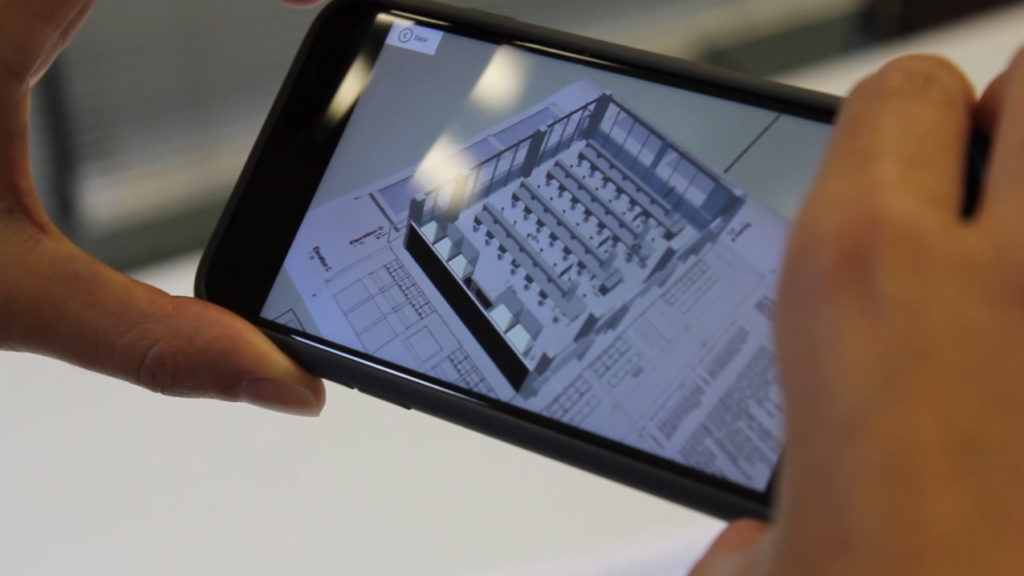
Options include immersive visualisation and virtual reality where you can put on a headset and literally walk around your new building months before construction even starts. This approach can transform the effectiveness of healthcare facilities, long before they are built. Even better, it will also inform the operational management of buildings and can test many options from infection control and social distancing to lighting and environmental factors.
Furthermore, remembering how important flexible spaces will be in the future, we will be able to see how rooms would look based on the different scenarios that the Covid-19 pandemic may bring.
