The flexible approach to estate design
Adrian Powell, Head of Property Development and Simon Taylor, Head of Portfolio Optimisation at NHS Property Services, outline the organisations evolving response to the pandemic.
During the peak of the pandemic and now amidst the second wave, the health service has had to swiftly expand its capacity to meet the increase in hospitalisations. As property advisors and owners of 10 per cent of the NHS estate, NHS Property Services played a role in finding and preparing clinical space for rapid deployment, with more than 1,000 additional beds being made available in our properties during this challenging period.
Now that we have seen a significant surge in cases, with virus hotspots across the country, we must gather and utilise our learnings from the past six months to support the NHS in managing and maintaining excellent patient care across all regions once again. This may be achieved through repurposing existing space or developing new, temporary structures that allow the NHS to treat both Covid-19 and other ailments. A one-size-fits-all approach is not suitable, so we must prepare to apply a local approach; one that addresses ever-changing customer needs and government guidelines.
The size of our estate portfolio has enabled us to have national specialist functions that support regional and local teams with technical input. This blend of national, regional and local teams helps to enable swift delivery, scaling up and efficiency through continuous learning and improvement. Collaborating with NHS England and Improvement (NHSE&I) has also been essential in allowing the health service to be flexible in the way it delivers care.
Over the past six months, working alongside NHSE&I has been key to providing use of vacant space and extending facilities management services. Our teams have addressed 350 additional space requests from our customers during this time. For properties that needed extra capacity during the first peak of the pandemic, all possibilities for creating space within the local area needed to be explored. For example, a health clinic in East Sussex requested support in building a temporary Covid-19 facility on a nearby acute site. However, after an assessment of needs and requirements, an alternative, unused site nearby was deemed more suitable given their rise in cases and short turnaround time. This allowed our teams to focus on repurposing space, creating a shower room, “hot” and “cold” zones, and new access routes for patients, all within three days. The result gave clinicians additional facilities in which to treat patients with symptoms, and took pressure off the nearest hospital.
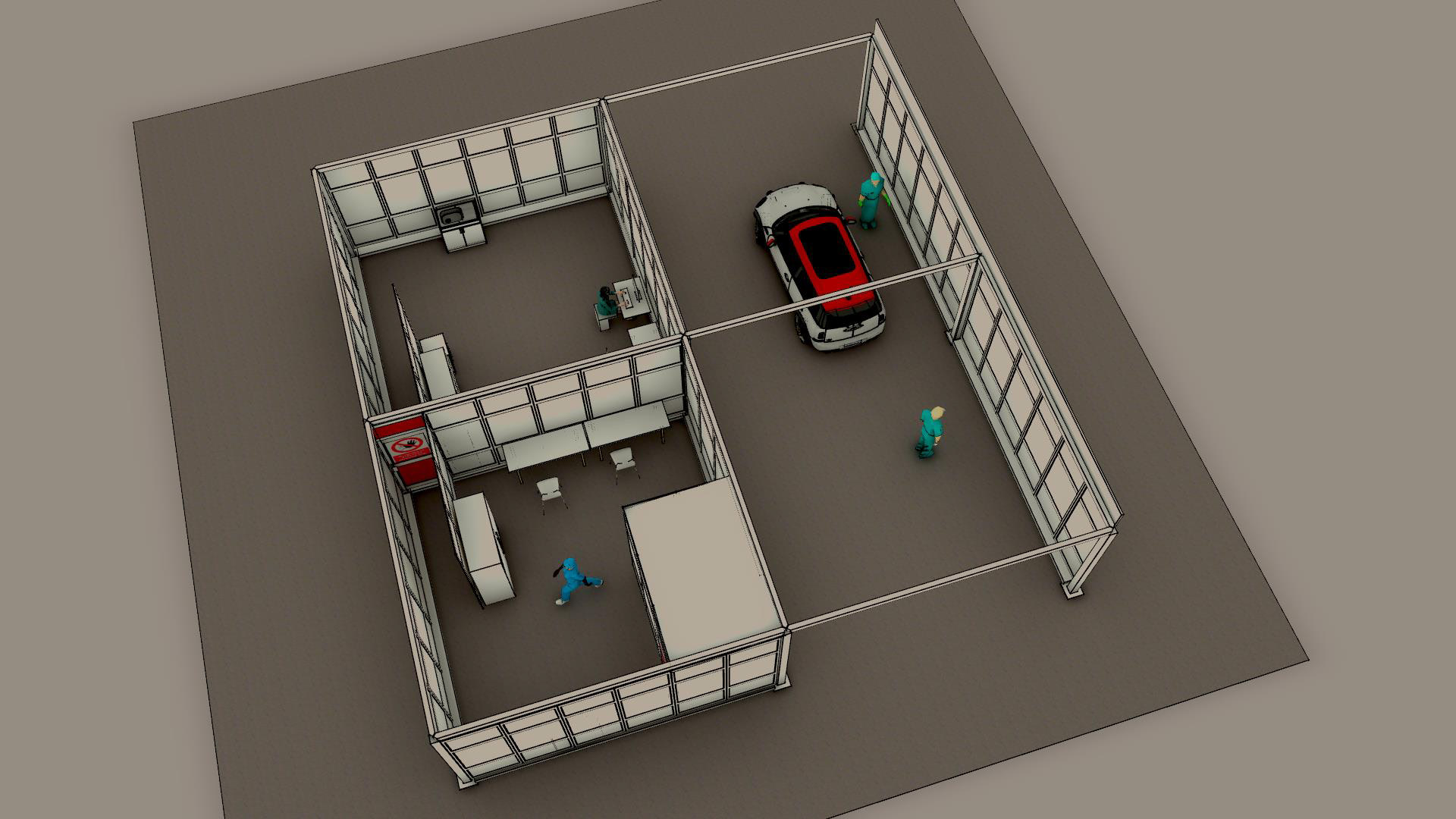
In addition to working closely with NHSE&I, we must also learn from our success in deploying a dedicated project team for regional requests. Through collaborating in this way, we can provide swift project implementation tailored to the local system’s clinical needs. As an example, our project team was able to work with Lancashire & South Cumbria NHS Foundation Trust to support it in finding additional bed capacity for Covid-19 patients and set up a community base for nurses to conduct Covid-19 testing for vulnerable patients, as well as a mobile testing clinic (pictured above) that would also serve the local area.
The project teams spanned facilities and asset management, construction, legal and health and safety, ensuring all aspects of the end-to-end delivery were efficiently carried out. Having a dedicated team when requests come in allows projects to move quickly, while ensuring they meet infection guidelines. This is particularly important when there are short turnaround times to get facilities up and running.
While we have learnt much from recommissioning or reconfiguring vacant or underused space across the estate, we need to ensure that we can add additional structures quickly – faster than the traditional construction delivery route. Temporary or modular buildings are an obvious choice for this, due to their quicker lead-in time, delivery and the Covid-response relaxation in town-planning requirements alongside the extension of permitted development rights to include them.
Where extra capacity is needed in community health services, modular buildings are useful assets that can be used to build additional capacity or separate services within local hospitals. As we see a rise in cases, and with uncertainty on when Covid treatment will no longer be needed, we need to ensure that essential hospital services are not impacted. For example, building a temporary structure that will allow for specific hot and cold areas, separating patients requiring treatment for Covid-19 symptoms and those not presenting symptoms and requiring other medical care. We also need to consider that, as we go back to the resumption of “normal” clinical service provision, the NHS will have many procedures returning, such as elective surgery and treatments that require overnight stays in hospitals. This is where we see modular building becoming an important option for additional space as it could provide safe new environments, including everything from bedded wards and shower blocks to diagnostic facilities.
As winter approaches, it is more important than ever that we support our NHS colleagues in preparing for the additional pressures of the colder months ahead. Drawing on our experience from the first wave, we are ready. Ready to reconfigure space, ready to assist local trusts with their requests and ready to set up buildings in the required timeframe. As capacity needs change, we will too. By continuing to be flexible in our approach and supporting customers, we will help support our clinical colleagues to deliver world-class healthcare.
