UK cancer patients waiting longer for treatment than comparable countries, research finds
Research compares access to radiotherapy and chemotherapy across four countries and eight cancer types.
New research by University College London reveals that cancer patients in the UK wait longer for treatment compared to several other nations. In a first-of-its-kind study, researchers analysed data from two studied published in the Lancet Oncology, covering more than 780,000 patients diagnosed with eight different types of cancer between 2012 and 2017 in the UK, Australia, Canada, and Norway. The cancer types were oesophageal, stomach, colon, rectal, liver, pancreatic, lung and ovarian cancer.
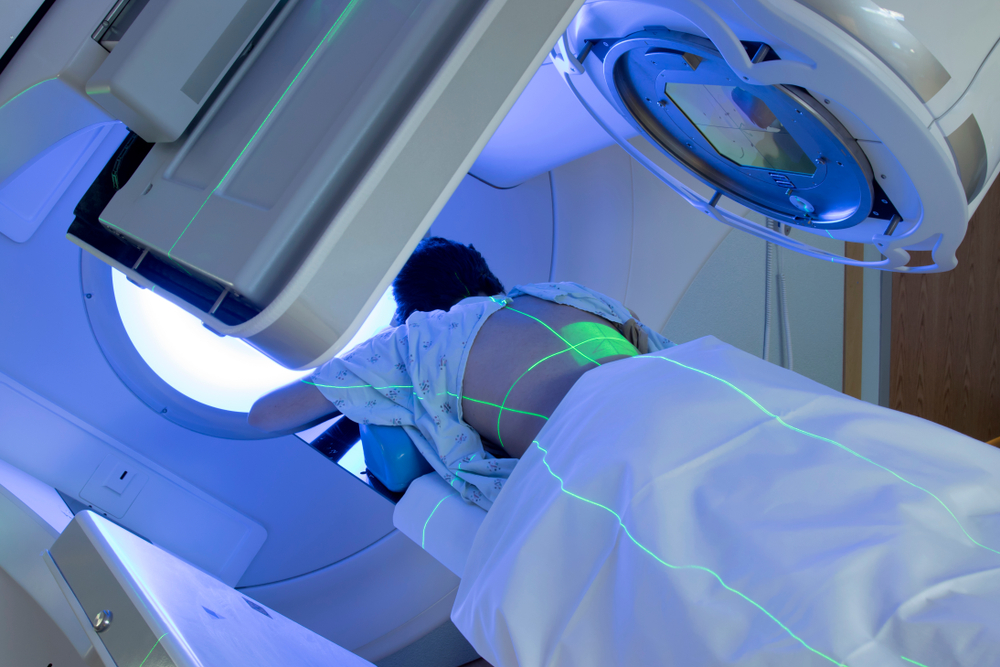
The study found that UK patients had the longest average waiting times for both chemotherapy and radiotherapy across all four countries. The average wait for chemotherapy in the UK ranged from 48 days in England to 65 days in Scotland, while Northern Ireland and Wales fell in between. Norway had the shortest average wait at 39 days.
For radiotherapy, the wait times were even longer in the UK, ranging from 53 days in Northern Ireland to 81 days in Wales. Newfoundland, Canada, had the shortest average wait at 42 days, followed by Northern Ireland (11 days longer), England (three weeks longer), and Scotland and Wales (seven weeks longer).
The study also highlighted that a lower proportion of UK patients with certain cancers received chemotherapy and radiotherapy compared to the other countries. For example, only 59 per cent of ovarian cancer patients in the UK received chemotherapy, compared to 73 per cent in Australia, 72 per cent in Norway and 67 per cent in Canada.
Similar disparities were observed for pancreatic cancer patients, with UK pancreatic cancer patients the least likely to receive chemotherapy or radiotherapy (27 per cent), compared with Canada (41 per cent), Norway (44 per cent) and Australia (47 per cent).
While not all patients require these treatments, chemotherapy and radiotherapy are key treatment options for cancer. The research suggests that countries with better cancer survival rates tend to have shorter waiting times and more frequent use of chemotherapy and radiotherapy. Cancer Research UK, which partly funded both studies, attributed the delays in treatment to a lack of long-term planning for cancer care in the UK compared to countries with strong cancer strategies and allocated funding.
This research offers valuable insights into the current state of cancer treatment in the UK and raises important questions about potential improvements to benefit patients.
Michelle Mitchell, Chief Executive of Cancer Research UK, attributed part of the UK’s poor performance on cancer treatment to the NHS’s longstanding workforce challenges, saying: “When it comes to treating cancer, timing really matters. We can learn a great deal from other countries who have stepped up and substantially improved cancer services. With a general election on the horizon, the UK government has a real opportunity to buck the trends we see in this research and do better for people affected by cancer.”
Cancer surgeon and Clinical Lead for the International Cancer Benchmarking Partnership, Dr John Butler, said: “Lower use of chemotherapy and radiotherapy in the UK could impact people’s chances of survival, especially for older patients. This study captures missed opportunities for patients in the UK to receive life-prolonging treatment.”
The Department of Health and Social Care said it has invested substantial sums into cancer care since the period covered by the research, citing £162m invested into radiotherapy equipment and £2.3bn invested into community diagnostic centres.
