Flow beats capacity: how we must change our hospital design

Terry Young, Emeritus Professor at Brunel University London and Director of Datchet Consulting, writes for Hospital Times and suggests how technology could be used better to improve hospital design.
We are still adding capacity for emergency provision and closing smaller sites to pay for it. Why is this still happening and how can we turn it around?
20 years ago, two groups used computer models (Lane, et al., 2000) (Wolstenholme, 1999) to show how extra hospital capacity would always fill up, whereas streamlining patient discharge would increase the number treated. Bluntly, their recommendations were for better solutions at the exit, instead of more capacity at the entrance.
“The overflow problem in urgent care is not primarily clinical or financial: it is about design”
Nonetheless, the NHS has invested heavily in extra urgent care capacity on the hospital frontline so that the UK now has 225 Acute Medical Units (AMUs) across its 152 acute trusts (according to NHS Confed statistics). Clearly, AMUs are a wonderful medical idea, but they are not the way to increase access or shorten waiting times in accident and emergency departments. The overflow problem in urgent care is not primarily clinical or financial, it is about design. We know that if we invest in capacity, our flow will never be far from crisis.
Healthcare delivery is a knowledge problem
Providing healthcare to millions of people is best thought of in terms of knowledge, rather as Sun Tzu saw war as an information challenge. Clearly, without good diagnosis and treatment, care is ineffective or worse, but millions die globally even though someone somewhere might have had the knowledge to treat and enable patient recovery. So how can we connect our knowledge to where it is needed most?
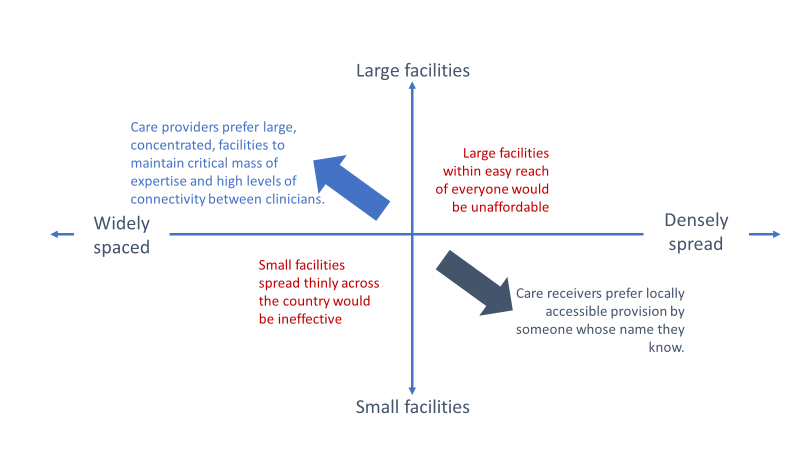
The above figure illustrates a knowledge paradox. Providers need people with specialist knowledge: the better and more complex the care on offer, the larger the provider community. Thus, hospitals are inevitably large, and will keep growing as the communities they serve grow and their needs grow more complex. Big hospitals are expensive, so we must spread them out.
However, those receiving care prefer localised services within easy reach and would like an expert who knows their name. This type of knowledge really does need something on every street corner.
Breaking the knowledge paradox
The primary-secondary care partition was an early attempt to address this paradox. However, when the internet changed what we knew about information and geographical separation, the healthcare dream became a possibility: a huge knowledge community within striking distance of anyone.
Again, about 20 years ago, the NHS set out with the National Programme for IT (later, Connecting for Health) to link the NHS’s major care provision facilities. However, the information solution was not tried and tested. It was deemed too difficult to use and later the programme was abandoned (with a nod to Chesterton).
It is interesting that Walmart, which viewed selling as an information challenge, managed to connect its suppliers and recast its knowledge paradox in retail about a decade earlier. The cost and complexity were not a million miles away from those faced in the project that the NHS closed, so it is tempting to ask why this knowledge was not made to work.
We have known about flow and capacity for a long time and have had a clear analysis of hospital systems since at least the start of the millennium (with models of wards etc., for a few decades before that). We know how to make flow work, much of it learned in the 1980s and 1990s in other sectors. Those sectors, too, have their knowledge paradoxes but have found their way around them.
End of the road for hospitals?
It is certainly not the end of the road for hospitals. The tools we need to prototype new service concepts and design the smallest details of flow along patient pathways already exist and have all been reported somewhere. The underlying principles of how systems work and what the knowledge economy looks like in other sectors have been clear for some time. Design tools and information infrastructure are not optional extras, they are foundational concepts.
Let’s stop building onto hospital entrances and make the exits smarter. Let’s stop counting beds and start measuring the knowledge envelope. Let’s call a halt to improvement and say hello to design.
References
Lane, D. C., Monefeldt, C. & Rosenhead, J. V., 2000. Looking in the Wrong Place for Healthcare Improvements: A System Dynamics Study of an Accident and Emergency Department. The Journal of the Operational Research Society, 51(5), pp. 518-531.
Wolstenholme, E., 1999. A patient flow perspective of UK health services: exploring the case for new” intermediate care” initiatives. System Dynamics Review, 15(3), pp. 253-271.
