Leveraging mobile technology to create systems of care that scale

Cynthia Bradford Lencioni, EVP Global Business & COO at Pulsara, illustrates how healthcare systems are removing traditional barriers to healthcare communication.
While tackling situations of untold pressure, the ability of healthcare professionals to deliver life-saving care is too often hampered by communication barriers. For instance, paramedics requesting an air ambulance are often faced with a cumbersome process of communication as the various regional command centres coordinate to secure a helicopter. An absence in real-time centralised communications among these sites can often result in fractured communication, needlessly delaying patient treatment at critical moments and impacting the quality of care.
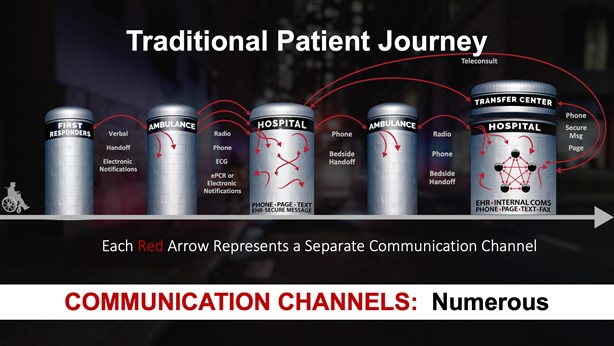
These scenarios are, unfortunately, all too familiar to those who provide prehospital critical care and indeed all those responsible for hospital care. From the missed radio report, to the page sent to the wrong team member, to the time spent not knowing whether the cath lab is ready for your patient – the disjointed nature of communication across hospitals can contribute to fragmentation, delays, and breakdowns.
The patching together of traditional, fragmented healthcare communication channels that open and close during a patient event—radios, telephones, pagers, faxes, emails—causes inevitable delays that negatively impact patient care. One patient transfer alone can involve numerous and often redundant telephone calls, radio reports, and other communications, creating a repetitive, error-prone process where precious time is lost at a time when your most critically ill patients need it the most. It is very difficult, if not impossible, to create a shared consciousness or unity of effort for critical patient events using traditional communication channels. It is also challenging for care providers to create an accurate clinical picture via radio or telephone—a photograph of an injury is worth a thousand words.
As an industry, we focus on uniting data, often not in real time with patients’ continuity of care, resulting in fragmented communications failing to fully leverage modern technology when every second counts. We should be focusing on the team members, logistics, and the communications to actually unite the care teams around the patient’s needs, accelerating lifesaving care.
Integrated communication is key
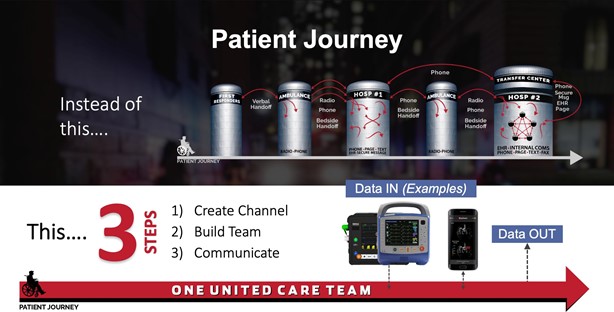
The solution to this problem is networked communication, powered by a rapid,
multi-directional flow of information, supported by interconnected mobile and online technologies. This can be accomplished by uniting the care team on a single, secure communication channel by means of creating a dedicated channel for a patient event and dynamically building the care team and adding teams, organisations, or individuals on the fly. Changing circumstances sometimes mean that additional team members, such as a specialist physician or mental-health provider, need to be added to the patient channel for a consult or collaboration. The result is a single source of truth for communication along with shared consciousness via the exchange of synchronous and asynchronous information—data, group messaging, live and recorded audio and video, images, exchange of facility capacity and readiness status, push notifications to all team members indicating alert acknowledgements, and transport ETA based on GPS. Nothing less than these capabilities will be able to unite and create situational awareness and shared consciousness for the entire care team.
In addition, the same networked communication will ensure that all care team members have shared consciousness around the patient’s outcome once definitive care is complete at the receiving facility, creating the ability to unify and inform all care teams in real-time as well as the necessary data for quality improvement and quality assurance review. It should be evident that when used to unite the care team across a system of care, a flexible communication and telehealth platform is unsurpassed in facilitating the level of complex care coordination across organisations and geographies that is required to ensure the highest quality of patient care in the shortest amount of time.
By uniting care teams for every patient event, networked communication enables systems of care that scale across time and geography. Whether for a patient case requiring a simple, 1:1 communication or a multi-region, multi-organisation event, such as a mass-casualty incident requiring one-to-many or many-to-many communication, a dynamic, interconnected communication system used each and every day for local, regional, and national stress events is a more-scalable system than traditional communication. The unique ability of such a system to bridge communication and coordination across all organisations participating in patient events, when surge events strain the system’s capacity, reveals its powerful flexibility and scalability.
Communication issues in healthcare are of course not exclusive to the UK. The communication crisis in healthcare is very much a global one where technology has, until recently, been a limiting factor.
Today, however, leading healthcare systems are creating improved risk and safety profiles by eliminating antiquated, non-integrated communication technologies. For example, Latrobe Regional Hospital, near Melbourne, Australia, replaced their outdated communication systems with networked communication and in so doing, was able to reduce treatment times for stroke patients by 68 per cent.
Instead of one-to-one, open and closed communication offered by radios, telephones, and pagers, networked mobile communication opens the door to one-to-many and many-to-many communications within patient channels. These channels can be created and used simultaneously and for the duration of the patient event. And in connecting previously siloed teams and organisations—in real time—networked communication supports faster, better coordination and the otherwise more difficult load balancing of available healthcare, transportation, and other emergency resources across Public Safety, Ambulance, Hospital, and Affiliated Healthcare teams within the system.
Time to treatment can be optimised and communication errors minimised, with the attendant quality and cost improvements that are demonstrated in the literature.

Systems of care that scale work for any patient method of arrival to the A&E (ambulance, walk-in, or inpatient) and for all time-sensitive emergencies. Any organisation, team, or individual can participate in a patient channel for communication that will enhance intra- and inter-organisational team communications. It is the resultant network, combined with the flexibility of the system, that allows the network to scale beyond routine interactions to enable all of the interactions and communication needed during a stress event. Enhanced communication has been proven to improve the time to assessment, transport, and treatment for critically ill patients.

The time is now for change
We can do more to help our healthcare providers to better prepare for the patient’s arrival by improving their visibility into the patient’s condition in the field. We can do more to facilitate the ability of facility staff and remote providers to collaborate on decisions about what care is needed and to determine whether and to which facility a patient’s transfer is most appropriate. We can do more to help healthcare teams to reduce medical errors and delays by reducing miscommunication. We can do more to provide opportunities for feedback that improve care.
The time is now for change in system planning, performance, and delivery to take a new view of leveraging mobile communications technology to unite distributed healthcare teams. In doing so, we will elevate the timeliness and quality of care for those in most desperate need, when seconds count. Higher quality at a lower cost will undoubtedly bring more value to any healthcare system that endeavours to make the best use of limited resources and achieve the Quadruple Aim.
