Uniting clinical and social care through IoT transformation

Peter Glover, Clinical Lead for Proactive Care, Farnham Integrated care in NHS North East Hampshire and Farnham CCG, outlines how digital could form the basis for health and care integration.
Coronavirus has presented huge challenges on a global scale, the economy has suffered, jobs have been lost and many businesses have borne the brunt as they run into significant financial difficulties. But these are all things that can recover. Sadly, the hundreds of thousands of lives that have been lost will not.
This is not to discredit frontline workers who have battled in vain to save thousands of lives, they have truly earned their hero titles and without these tremendous efforts, it’s safe to say thousands more lives would have been lost.
There has been no choice but to rely upon digital solutions to cope with the extra pressure – a move long overdue, but nonetheless, welcome. This digital evolution within the healthcare sector must continue beyond the Covid-19 crisis and crucially, clinical and social care must be much closer aligned to deliver better care for the population as a whole.
Building on experience
The issue of joining up patient clinical records remains a challenge. Too often, patients visiting different clinical settings, such as their GP, A&E or outpatient setting must repeat their medical history as clinicians do not have full access to medical history. For example, ambulance personnel called to complex, chronically ill patients need information to understand the baseline for that patient. Without it, the default must be to take them to hospital – a move that is counter-intuitive to the patients long term health given the risks of infection.
To combat this, an intelligence based information system (IBIS) was created that allowed community clinicians to upload relevant, precise, clinical information about their patients, and so if the patient dialed 111 or 999 that patient’s medical information would be unlocked, allowing for the best possible patient care and outcome. As a result, the ambulance service has been transformed far beyond a 2D model.
However, it is now time for the whole of the NHS to digitally change for the better, and not look back. Returning to ‘normal’ healthcare settings that rely on paper-based records post Covid-19 should not be a strategy.
No Looking Back
The strategy for moving forwards should be guided by digital tools such as risk analysis, AI and machine learning – these help empower clinicians with accurate and shared patient information in order to deliver a more holistic and meaningful approach to care. With a simple app on your phone and sensor attached to your thermostat within your home, it is possible to find out what temperature your living room is recording, and in turn it is possible to adjust the temperature to your preference without even being at home. It is this kind of smart technology that should be rolled out widely and applied to numerous functions across the social care setting, as it has the potential to transform the level of support given to our most vulnerable individuals.
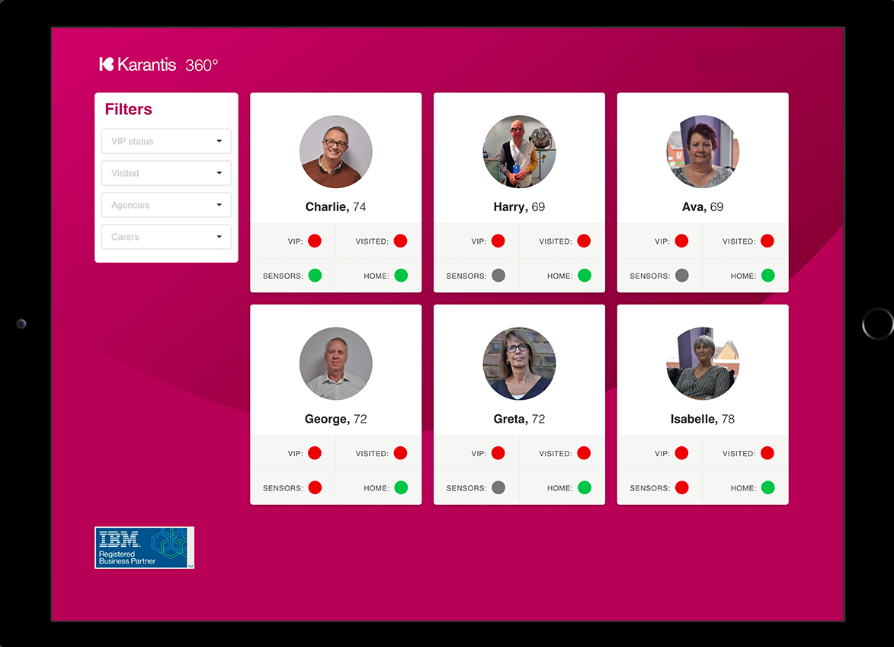
IoT systems like that of Karantis360 provide mobility to move from where we are now to where we want to go. By unassumingly monitoring movement, humidity, and temperature across a home enables a care organisation to rapidly gain a picture of each individual’s day to day routine – information that is then key to flagging changes which could reveal a problem. These AI based tools arm carers with better information and enable them to intervene at the right time and create a care programme that best suits the needs of the individual. This information also provides a platform for the end to end digitisation of healthcare, co-ordinating the ecosystem of local authorities, healthcare providers, NHS Trusts, GPs, registered nurses and care homes. This inspires a more proactive and interlinked approach to care.
In most cases of older and chronically frail patients, there are evidential and significant warning signs of deterioration. A person with a urinary tract infection (UTI), for example, may see an increase in the need to urinate while becoming slowly more agitated and irritated over a few days, their hydration level will decrease, their body temperature will increase, their appetite will decrease. Detecting early warning signs using at-home monitoring technology allows for intervention before the patient reaches a critical point, thus reducing the high emergency cost to the NHS, and most importantly improving the patient outcome.
Time for real change
The familiar saying ‘social care in crisis’ is nothing new, and it’s only been further exacerbated by Covid-19, but without implementing real change it will never go away. The time has come to acknowledge and embrace the power of digital technology, like what has already been witnessed across different sectors within the NHS since Coronavirus forced digital transformation – the ‘Test and Trace’ system or the new GP E-consult, for example.
The reality is that planned transformation often has many process and ownership barriers, and so a complete overhaul will take time. But, IoT and home-monitoring models, such as Karantis360, bypasses some of the industry barriers by going straight to the patient with a solution that can empower a vulnerable individual’s relatives, loved ones and caregivers, to ensure the individual has a full, meaningful, safe life in a place they choose, in a manner that they dictate.
